As healthcare increasingly moves toward a population health focus, marketing and communication professionals can play a crucial role. By learning, adapting, and applying evidence-based theories and models of behavior change, they can not only meaningfully participate, but perhaps even take the lead, in defining population health objectives and implementing strategies.
In fact, let’s push this notion even further and posit that the most effective approach involves marketing and clinical services working together in a collaborative model for behavior change.
Consider the contributions that marketing/communications and clinical team members (physicians, nurses, dietitians, pharmacists, physical therapists and the like) can each bring to the table: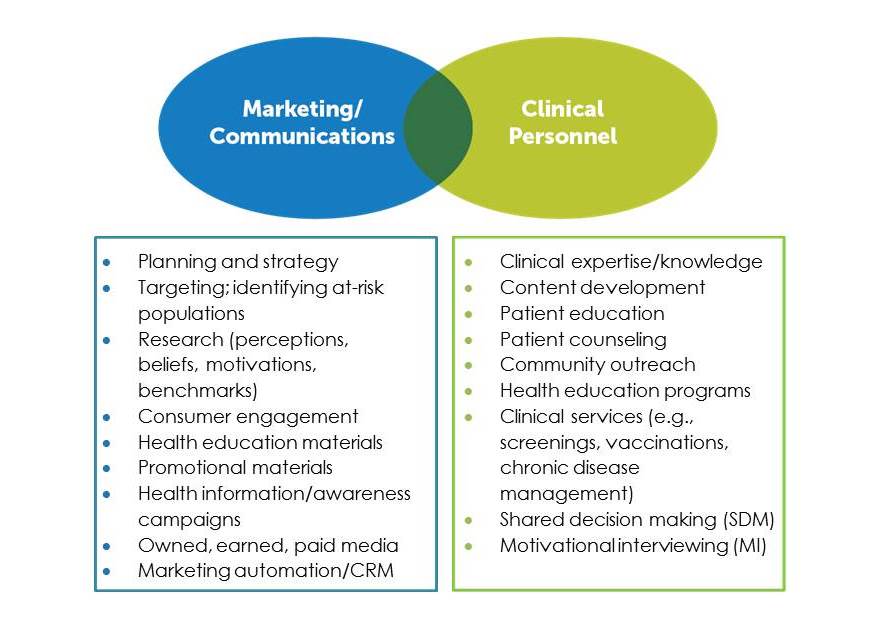 A collaborative approach to behavior change would bring these two sets of contributions together, for maximum impact.
A collaborative approach to behavior change would bring these two sets of contributions together, for maximum impact.
The Stages of Change Model
One model of behavior change that is ideally suited for such collaboration is the Transtheoretical Model, more commonly called Stages of Change (SOC). Developed by James Prochaska and his associates in 1977, SOC was designed to help at-risk populations adopt healthier behaviors by moving through a series of well-defined steps. This is accomplished by matching the individual’s stage—or state of readiness—with the appropriate message, media, and program for behavior change. SOC is at the heart of customer relationship management (CRM).
The six Stages of Change are: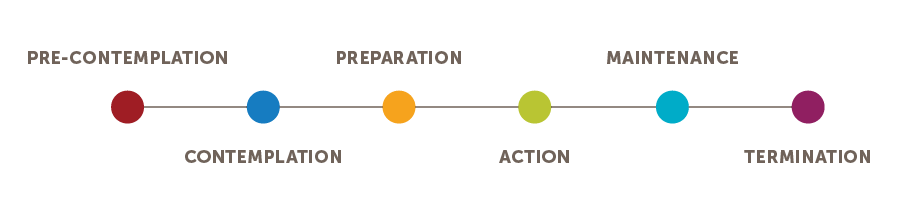
Precontemplation. The individual has no intention of making a behavior change in the coming six months. This may be due to lack of awareness (the health risks are not even on this individual’s radar) or demoralization (the individual has tried to make a behavior change in the past and failed).
Contemplation. The individual intends to make a behavior change in the next six months but is ambivalent—weighing pros and cons.
Preparation. The individual is ready to make a change in the coming month and is primed to take a first step, ranging from watching a video or attending a class to scheduling an appointment for a health screening.
Action. The individual has made a behavior change in the last six months that is sufficient to reduce the health risk.
Maintenance. The individual in this stage, which can last from six months to five years, must now focus on not relapsing or returning to the former unhealthy behavior.
Termination. The individual has fully adopted the new behavior as a well-established habit and has no risk of backsliding.
This model provides a solid framework for an effective behavior change program, which can be jointly executed by marketing and clinical team members. To strengthen patient engagement and further enhance efforts, Shared Decision Making and Motivational Interviewing can be incorporated :
• Shared Decision Making (SDM) is a process that involves two-way communication—with the clinician and the patient working together to explore various treatment options, including evaluating the pros and cons and the benefits and risks of each alternative. The patient is then able to make an informed choice that takes into account his or her own needs, goals, values, concerns, preferences, and life circumstances. The patient feels respected and empowered and, as a result, is more likely to follow through with the agreed-upon treatment plan.
• Motivational Interviewing (MI) is a style of communicating that is specifically designed to elicit behavior change. The clinician conveys empathy and facilitates movement by acknowledging the patient’s feelings of ambivalence about change, mobilizing the individual’s values and goals, and activating their own reasons to change. Core skills of Motivational Interviewing are active listening, asking open-ended questions, and reflecting back what the patient is saying and feeling.
Stages of Change in Action
The following chart illustrates a Stages of Change campaign in action. The goal is to encourage low-dose lung cancer screenings for long-term, heavy smokers.
Everyone Benefits
When marketing and clinical services collaborate and deploy evidence-based behavior change models and techniques—such as Stages of Change, Shared Decision Making, and Motivational Interviewing—everyone benefits:
• Marketing and clinical goals and objectives are aligned
• Resources are focused and less fragmented
• Messages and response mechanisms are in sync with consumers’ stages of readiness
• Patients are engaged and more likely to adhere to treatment plans
• Better clinical outcomes are achieved
• Customer satisfaction is higher
Creating a collaborative model for behavior change doesn’t happen overnight, and you may experience some resistance. But more often than not, clinical colleagues will welcome the very specialized support that marketing can offer—from strategy and research to implementation of CRM campaigns. Behavior change and health improvement in a population health environment are shared responsibilities, and everyone has an important role to play.
Learn more! Exclusive benefit for Forum Members: Check out Susan Dubuque’s session (with Katie Mardigian and Heather Valentine) from the 2018 Healthcare Marketing & Physician Strategies Summit.

Susan Dubuque has studied, researched, and written extensively on the subjects of population health and behavior change. She is a principal and co-founder of ndp, a marketing and advertising firm based in Richmond, VA, and an adjunct instructor at Virginia Commonwealth University in the School of Healthcare Administration.
Eileen Myers, MPH, RDN, LDN, CEDRD, FAND, a Nutrition Expert and Registered Dietitian Nutritionist, also contributed to this article.


